An Australian man with heart failure has become the first person in the world to survive more than 100 days with an artificial titanium heart as he waited to receive a donor transplant.
The breakthrough raises hopes that fully mechanical hearts could one day replace the need for donor transplants.
Diseases of the heart and surrounding blood vessels are the leading cause of death globally, killing about 17.9 million people each year, according to the World Health Organization.
Here’s what to know about how the titanium heart works, and whether it can solve the global donor shortage.
What happened with the man with an artificial heart?
The man in his 40s, who declined to be identified, became the first person to be discharged from hospital with a fully artificial heart implant.
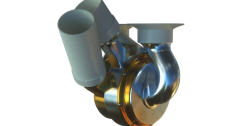
During a six-hour surgery in November 2024 at St Vincent’s Hospital in Sydney, the BiVACOR Total Artificial Heart (TAH) made of titanium was implanted into the patient, who was experiencing severe heart failure.
After spending a few weeks in intensive care, followed by observation in the hospital, the patient was discharged in early February.
He lived with the artificial heart for 105 days before receiving a donor heart transplant on March 6, and is currently recovering well, according to his doctors.

Has anyone else had a titanium heart transplant?
In July 2024, a 57-year-old man with end-stage heart failure received the BiVACOR TAH at Baylor St Luke’s Medical Center in Houston, Texas in the United States.
This was the first human implantation of the titanium heart, serving as a bridge to a real heart transplant. The device supported the patient for eight days in the hospital until a donor heart became available.
Between July and November 2024, four other men in their mid-40s to mid-60s in the US also received the BiVACOR TAH. Each patient successfully transitioned to a donor heart transplant and was discharged from the hospital within a month. None of the US patients left the hospital with the device.
Could it solve a heart donor shortage?
The titanium heart could possibly help address the donor shortage by keeping patients alive while they wait for a real heart transplant. Additionally, not everyone with heart failure is eligible for a human heart transplant in the first place due to factors such as old age, underlying conditions, or substance abuse. Donor hearts are typically reserved for those with the most serious cases.
Although it is still unclear whether the titanium heart could ever become a permanent replacement, experts on the team say that is their ultimate goal.
“While we are starting with a cohort of patients who are clinically declining while awaiting heart transplant, the more important patient population is the group of patients who do not have transplant as an option,” said Joseph Rogers, president of the Texas Heart Institute and national principal investigator for the US trials.
The US procedures began as a five-person early feasibility study approved by the country’s Food and Drug Administration (FDA), with plans to expand to 15 more patients in the coming months. These trials aim to determine whether the titanium heart can safely keep patients alive while they wait for a transplant.
After this phase, Rogers says the team plans to launch a larger study that will also include patients who may accept the BiVACOR heart as a permanent replacement for a failing heart.
“If all goes well with the clinical trials, I could imagine the device being available more globally in 4-5 years,” he told Al Jazeera via email.
Still, he adds that people must take care of their heart health so that they never need any of these therapies.
The need for alternatives like artificial hearts is because finding a donor heart isn’t easy – there aren’t enough available and matching a heart to a patient can take time. In the United Kingdom, for example, patients on the regular waiting list for a donor heart usually wait 18 to 24 months. Those in urgent or emergency cases get priority and may receive a heart sooner because their condition is more critical.
Heart failure affects at least 26 million people worldwide, including 6.2 million adults in the US. However, heart transplants remain rare, with fewer than 6,00